Provider Enrollment and Credentialing: Maximizing Efficiency in Healthcare
Understanding Provider Enrollment
Provider Enrollment is the process of getting healthcare providers like doctors and hospitals enrolled in insurance networks and government healthcare programs. It involves a lot of paperwork, checking credentials, and following rules to make sure providers meet the requirements.
Streamlining Provider Enrollment Processes
To make Provider Enrollment faster and easier, using technology is really important. Automated systems help with submitting applications quickly, verifying information faster, and reducing mistakes. By using smart algorithms, organizations can improve accuracy and speed up the process, saving time and resources.
The Significance of Credentialing
Credentialing is all about making sure healthcare providers are qualified and capable of giving safe and effective care. It involves checking qualifications, experience, and skills to maintain high standards and build trust in the healthcare system.
Enhancing Credentialing Efficiency
Traditional ways of credentialing are outdated. Digital platforms help organizations speed up the process, verify credentials faster, and meet regulations. Storing credentialing data securely online allows for easy sharing of information and improves transparency.
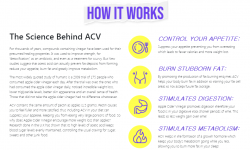
Leveraging Technology for Efficiency Gains
Technology plays a big role in making provider enrollment and credentialing services processes better. Blockchain technology helps keep records secure and prevents fraud in Provider Enrollment. Telecredentialing allows for remote verification of credentials, making it easier to onboard new providers.
Harnessing Data Analytics for Strategic Insights
Using data analytics gives healthcare organizations valuable information to make smart decisions in Provider Enrollment and Credentialing. Predictive analytics can predict trends, identify problems, and allocate resources efficiently. Real-time dashboards provide visibility into credentialing workflows, helping stakeholders monitor performance and improve processes.
Embracing Collaborative Partnerships
Working together with third-party services and technology vendors can help healthcare organizations improve their Provider Enrollment and Credentialing processes. By partnering with others, organizations can speed up application processing, ensure compliance, and integrate innovative solutions for continuous improvement.
Cultivating a Culture of Continuous Improvement
Continuous improvement is key to making Provider Enrollment and Credentialing more efficient. By setting quality standards, measuring performance, and making targeted improvements, organizations can optimize their processes. Encouraging collaboration and sharing knowledge among stakeholders drives innovation and excellence in enrollment and credentialing practices.
Conclusion
Provider Enrollment and Credentialing are essential for the healthcare billing solutions system to work smoothly and deliver high-quality care. By using technology, building partnerships, and focusing on improvement, healthcare organizations can enhance efficiency and effectiveness in Provider Enrollment and Credentialing, ultimately improving patient care.